Attention Deficit Hyperactivity Disorder
Attention deficit hyperactivity disorder (ADHD) is one of the most common neuropsychiatric childhood disorders and can carry on through teenage years and later life. The average age of onset is 7 years old. Symptoms include difficulty staying focused, paying attention and Concentration, difficulty controlling behaviour, and hyperactivity (over-activity).
Prevalence
In India, the prevalence of ADHD among children was 1.7% in children less than 14 years of age. It is important to realize that ADHD persists in 50 to 80% of the affected during adolescent age. It was found to be higher among the males (66.7%) than that of females (33.3%). The incidence among the lower socio-economic group was 16.33% and that among the middle socio-economic group was 6.84%. The highest in the age group 9 and 10 years. Studies show that the number of children diagnosed with ADHD is increasing, but it is unclear why. ADHD causes significant functional impairments, such as social and family life problems, poor education and school dropout, low self-esteem, impairment in emotional development.
The main core symptoms of ADHD Inattention, hyperactivity and impulsivity.
To be diagnosed with the disorder, a child must have symptoms for six months or more months.


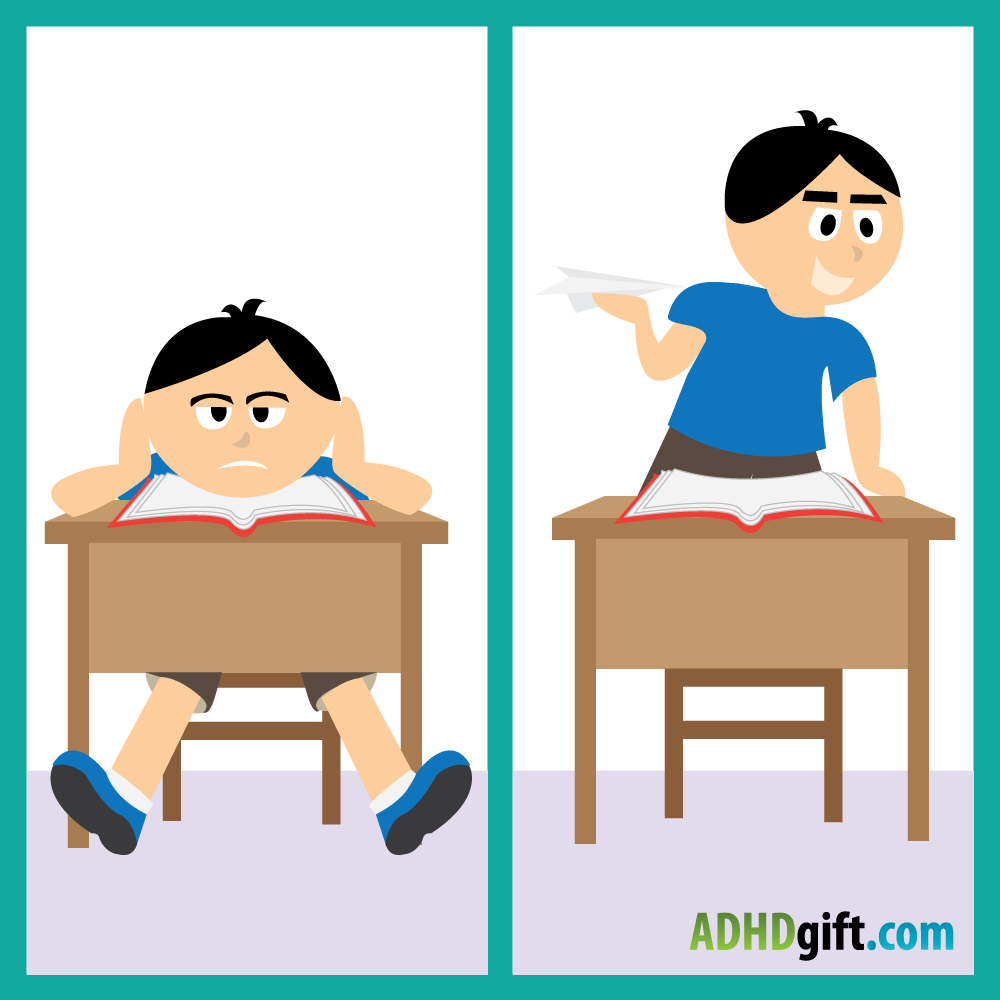
Symptoms of Inattention in Children
-Easily distracted
-Complexity in attention
-Switch from one activity to another
-Difficulty in focusing on one thing
-Struggle to follow instructions.
-Trouble in completing or turning in homework assignments
-Easily confused, and move slowly
-Become bored with a task after only a few minutes
Symptoms of Hyperactivity in Children
-Fidgeting
-Jumpiness
-Nervousness or excessive movement
-Difficulty in concentrating or focusing on a task
-Taking Nonstop
-Difficulty to remain quiet in school or to sit in one place
Symptoms of Impulsivity in Children
-Impatience
-Have difficulty waiting for things they want
-Act without regard for consequences
-Interrupt conversations or other activities
-Doing Dangerous activities
Co-Morbidity Disorders:
-Oppositional defiant disorder (ODD)
-Conduct disorder (CD)
-Anxiety
-Depression
-Bipolar disorder (BPD)
-Substance abuse.
Co-Morbidity Disorders:
-Oppositional defiant disorder (ODD)
-Conduct disorder (CD)
-Anxiety
-Depression
-Bipolar disorder (BPD)

Investigations and testing:
Following tests can be done only if indicated and relevant –
-IQ and academic assessment
-Speech and language assessment
-Social development evaluation and pre-vocational skills assessment
-Neuropsychological tests – not required as part of the routine assessment for ADHD
Treatment and Management
-Pharmacotherapy
Psychosocial Interventions
Behaviour therapy with child and Parent Management Training (PMT)
Behaviour Therapy
Behaviour therapy is a technique to improve parenting skills and a child’s behaviour. Behaviour therapy focuses on specific problem behaviours by structuring time at home, establishing predictability and routines, and increasing positive attention. In behaviour therapy, two kinds of behavioural interventions can help children with ADHD manage their symptoms of hyperactivity, impulsiveness, and inattention. There are two techniques, positive reinforcement (rewards chart, token economy, praising, time out) and negative reinforcement (punishment or taking pleasurable activities). Parents can use both techniques depends upon the child behaviours.


Parent Management Training ( PMT)
Parent management training (PMT), also known as behavioural parent /training (BPT) or parent training, is a family of treatment programs that aims to change parenting attitudes and behaviours, teaching parents positive reinforcement methods for improving pre-school and school-age children’s behaviour problems (such as aggression, hyperactivity, temper tantrums, and difficulty following directions)
“These positive reinforcement techniques (such as praise, smiles, and hugs), as well as concrete rewards (such as stickers or points towards a larger reward as part of an incentive system created collaboratively with child), can be useful for any child with disciplinary problems”.
Family therapy
ADHD is also treated with various psychosocial and psychoeducational interventions for parents, children, and multicomponent interventions combined with medication management. Family therapy may help families cope with distress from the presence of the disorder. Parents should first regulate their parenting style. Using something called “Family Dynamics” & six types of parenting styles, including Teacher, Supporter, Moulder, Guide, Dependent and the Monarch. Each of these styles works differently to deal with ADHD children, and each parent must know their strengths and weaknesses. The success of any therapy is determined by the people’s willingness to seek more protective behaviour. All members of the family must be willing to change their behaviour patterns to promote change.


Social skills training
Social skills training is one of the treatments that help children identify and address social problems. It is usually done in group therapy. The training helps the child with (ADHD) be less aggressive and impulsive, manage anger, and behave in a more socially acceptable manner with a specific step-by-step approach. Techniques include:
-Roleplay and rehearsal
-Watching videotapes of positive behaviour
-Practising ways to resolve conflicts
-Listen and engage in conversation – Classroom and social gatherings
-Enter new group situations
-Give and receive praise and criticism
-Cope with frustration
Remedial education – if Needed (For Academic difficulties)
Remedial education is very important for ADHD children. They are frequently involved in conflicts with peers and teachers, and they are regarded as a bully and disturbing. Their troubles to focus often result in inattentiveness, and when the teachers give instructions to the class, their thoughts are usually somewhere else. They miss a lot of information taking notes in class. The parents and teachers may face difficult to control their behaviours in schools and homes.
So due for this reason, Special Education is needed for these children. Every ADHD child is unique in their behaviours. Remedial education is depended upon the level of child functioning. The special educators are skilled to treat them. They use different types of remedial teaching techniques to treat them.
Certain techniques are
-Psychoeducational training for parents.
-Behaviour Modification training.
-Improving academic activities – Coping with school curriculum (overall).
-Teaching special techniques to remember their subject.
-To Improving organizational and language skills.

Occupational therapy — if required
-Certain techniques are Control their “energy” levels, hyperactivity, etc.
-Activities to work out anger and aggression.
-Improving daily living activities – like brushing teeth, bathing, getting dressed, or feeding him or herself, taking care of personal things.
-Practising handwriting and hand co-ordination.
-Physical co-ordination.
-Play games, such as catching or hitting a ball to improve co-ordination.
-Works on Time management.
-Control their “energy” levels, hyperactivity, etc.
-Activities to work out anger and aggression.
Improving daily living activities – like brushing teeth, bathing, getting dressed, or feeding him or herself, taking care of personal things.
-Liaison with Special School.
-Refer to Support groups.