Depression
Termed as Major Depressive Disorder, one of the commonest psychiatric disorder. Ranks as 2nd causes of disability worldwide just only to heart disorders. As with other medical disorder, depression carries significant morbidity and mortality.
Not only suicide-a major concern, a depressed person won’t be able to carry out his routine work and will land-up with difficulties with interpersonal relations.
History
The earliest documents account for demon & evil spirits as the case of depression. Hippocrates, the father of medicines attributed mental illness to imbalance in four body fluids called human- yellow bile, black bile, phlegm and blood. Melancholia Depression was attributed to excess black bile in spleen.
Robert Burton published a book “Anatomy of melancholia” in which he analyzed both social& psychological cause of depression such as paranoid, fear & loneliness- this theory still holds good even today.
In the 19th century Emil Kraepelin introduced biological cause to mental illness and coined manic depression. Later psychoanalysis, cognitive & behavioral theories became popular.
20th century revolutionized the understanding the sociological causes of depression and an array of medicines to cure depression was discovered.
Ancient vedas, upanishads, Ramayana & Mahabharatha give vivid description of depression. Yogavasishtam written by sage Vasishtar describes vividly about Lord Rama’s adolescent crisis , despondency and depression. Bhagavat gita is the oldest, documented crisis intervention & counseling in the world.
Lord Buddha, Mahaveera and many sages explained in depth about depression, sorrow & were of the opinion that desire is the root cause of all evils.
Is depression a disorder or the affected person just lack coping skills or is he mentally weak?
Depression is not a weakness. It is biological. It can appear OUT OF THE BLUE without any event. Or it can manifest due to severe life stress. It is not about coping skills. The mental pain the patient suffers is REAL and can only be described by him. Like all Medical disorders such as infections, Hypertension, Diabetes it can be treated with medications and person can be completely back to normal functioning.
What is the difference between sadness & Depression?
If there is a real loss of loved objects (death of a family member, pet animal) or sickness in the family, failing in selection, it is normal to be sad. It is also normal that he should cope up with himself & return to reality. If this sadness exceeds beyond 2 weeks and interferes with his duties then we call it as depression.
Who gets Depression?
- Depression can occur to anyone, but it is twice common in female than male.
- Usually affects middle age 25-45 years, but recent years children, adolescents and elderly are commonly affected.
- All social status, irrespective of religion, cast and income
- Equally in rural and urban population
- More frequently associated with co morbid medical or neurological illness example with thyroid dysfunctions, Parkinson’s disease, Stroke.
- As secondary to dysfunction and disability caused by chronic medical illness like post myocardial infarction, cerebrovascular accident (stroke), cancer, arthritis.
- Following longstanding psychiatric illness like schizophrenia, alcohol use disorders
How common is Depression?
- Approximately one of every five can get depression in their lifetime.
- At one point of time at least 10% of the population is suffering from Depression but less than 20% get treatment for it.
- Depression is found in 30-40% of Out-Patients attending primary care and other consultants.
- Depression is still more common in patients with chronic medical disorders like cancer, Diabetes, Cardiovascular disorders, Arthritis, autoimmune disorders ect.
- Even the care givers of patients with chronic medical or psychiatric disorders are found to have depression.
Depression: DSM-5 Diagnostic Criteria
The DSM-5 outlines the following criterion to make a diagnosis of depression. The individual must be experiencing five or more symptoms during the same 2-week period and at least one of the symptoms should be either (1) depressed mood or (2) loss of interest or pleasure.
- Depressed mood most of the day, nearly every day.
- Markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day.
- Significant weight loss when not dieting or weight gain, or decrease or increase in appetite nearly every day.
- A slowing down of thought and a reduction of physical movement (observable by others, not merely subjective feelings of restlessness or being slowed down).
- Fatigue or loss of energy nearly every day.
- Feelings of worthlessness or excessive or inappropriate guilt nearly every day.
- Diminished ability to think or concentrate, or indecisiveness, nearly every day.
- Recurrent thoughts of death, recurrent suicidal ideation without a specific plan, or a suicide attempt or a specific plan for committing suicide.
- To receive a diagnosis of depression, these symptoms must cause the individual clinically significant distress or impairment in social, occupational, or other important areas of functioning. The symptoms must also not be a result of substance abuse or another medical condition.
- The patients do not present to the clinician exactly with the above set of complaints- a suspicion of depression should be raised when patient present with
Depression should be suspected when a person who withdraw oneself from his/her social surroundings, or when there is a sudden decline in academic performance in a child or adolescent, or a change in behavior in an elderly person.
It should be always screened in patients with long standing disease and in postpartum women.
Why it should be diagnosed?
As said earlier, a depressed individual cannot concentrate in his work, the lack of pleasure, the fatigue and other symptoms causes decline in social and occupational functioning.
This leads to decrease in productivity and piling up of such symptoms lead to reduced social well being in the society.
Even in medical settings, diagnosis and treatment of co morbid depression is important.
Studies have proved that presence of depression affects the prognosis of the medical disorder both in morbidity and mortality.
For example a post Myocardial infarction (MI) patient with depression has increased chance of next MI, even if he is compliant to all cardio protective drugs. And it has also been proved that treatment with antidepressants have prolonged the survival of these patients.
Risk factors for Depression
Genetic factors– family history of Depression
Childhood experiences
- Loss of parent at young age, lack of parental care, parental alcoholism/antisocial traits, childhood sexual abuse.
- Social circumstances-
- Unmarried (in male), married women with marital disharmony, widowed, living single, divorced individuals
- Interpersonal conflicts, lack of confiding relationships, lack of support
- Social stressors: unemployment, communal disharmony, famine, migration, natural disasters like flood, earthquake..,
- Decline in global economy due to “Pandemic” like COVID 19
Physical illness
Cardiovascular diseases, neurological disorders like Stroke, Parkinson’s, Endocrine disorders like Hypothyroidism, Addison’s disease, Cushings syndrome, Autoimmune disorders like Rheumatoid arthritis, SLE, Malignancy, Disabilities due to bone fractures, limb deformities, Renal conditions like Chronic Renal failure.
All the above can cause loss of productivity, increasing cost of treatment, availability of support system, and medical facilities leads to Hopelessness, Helplessness and Depression.
Depression at various stages of life
Childhood depression
- Up to 5% of children experience clinical depression.
- Children with depression may appear persistently sad, may no longer enjoy activities they normally enjoy, or they may frequently appear agitated, or irritable. They cry even for very sillyissues
- Depressed children may frequently complain of physical problems such as headaches and stomach aches and often have frequent absences from school or poor performance.
- They may appear bored or low in energy and frequently have problems in concentrating.
- A major change in eating or sleeping patterns is a frequent sign.
- Children under stress (like parental dispute, father’s alcoholism, change of residence, change of school), who experience loss, or who have learning disorders are the important risk factors for depression.
Adolescent Depression
Adolescence, transitional phase of growth and development between childhood and adulthood
The World Health Organization (WHO) defines an adolescent as any person between ages 10 and 19 years. They have high frequency of emotional disturbances, mood lability, and low frustration tolerance, easily rebellious and behavioral experimentation.
Recent studies have shown that greater than 20% of adolescents in the general population have emotional problems and one-third of adolescents attending psychiatric clinics suffer from depression.
Depression presents in adolescents with essentially the same symptoms as in adults
- Pervasive sadness may be exemplified by wearing worn out dresses, writing poetry with morbid themes or a preoccupation with music that has nihilistic themes.
- Sleep disturbance may manifest as all-night television watching, excessive mobile use, gaming addiction, difficulty in getting up for school, or sleeping during the day.
- Lack of motivation and lowered energy level is reflected by missing classes.
- Loss of concentration, slowed thinking and boredom may lead to academic decline.
- Loss of appetite may lead to anorexia or bulimia.
- Adolescent depression may also present primarily as a behavior or conduct disorder, substance or alcohol abuse.
- Pessimistic view of world, suicidal threats and attempts are common. Suicide is the leading cause of death among them.
Depression in middle age
- Depressed middle-aged adults are at four times greater risk for being unable to perform everyday tasks than their non-depressed colleagues.
- Depression during these ages is strong determinants for job loss, marital disharmony, divorce, substance use and suicide. Sexual dysfunction is also a presenting symptom of depression
- Marital problems, economic crisis that arise to fulfill needs of the family or children, physical illness in a family member, caring a elderly, a stressful job, alcohol use among one family member are the important causes of Depression in middle age.
Depression in women
Depression in women is twice common than men
Certain stress is unique in women such as;
- Coping with menstruation, pregnancy, and menopause
- Multiple roles such as a mother, a wife, a daughter-in-law, a professional.
- Frequent victim of violence and sexual abuse.
- In India it is customary for women to leave her maternal place following marriage, the new city or town, and the new individuals (In-laws) to cope with are some factors.
About half of new mothers find themselves sad, angry, irritable and prone to tears soon after giving birth. These feelings sometimes called the “baby blues” which is normal and generally subside within a week or two.
But if they don’t subside quickly, if symptoms are severe, if they’re accompanied by an inability to care the baby , refusing to feed the baby or thoughts of harming the baby, or having feelings of anxiety, low self-esteem, agitation, suicidal ideation are to be treated as “Postpartum depression (PPD)”.
Postpartum depression can occur in 2-5% of mothers
This isn’t merely a matter of being unable to cope with having a new baby; rather, it’s probably associated with major hormonal fluctuations that influence mood, as well as an underlying predisposition to depression. This is a serious psychiatric condition requiring prompt treatment to prevent Infant neglect, maternal suicide or infanticide.
Occasionally (0.1-0.2%) the mother can have delusions and hallucinations related to childbirth and infant known as “Post Partum Psychosis”, which is again a psychiatric emergency to be identified and appropriate treatment to be started at earliest
Depression in Elderly
Depression is the most common psychiatric disorder in the elderly population, 10-25% of people over 65 years suffer from significant depressive symptoms.
Depression, is frequently co-morbid with medical illnesses, has a negative impact on the quality of life, increases the number of visits to different medical services, and carries a high risk of suicide, especially in men. Despite these factors, depression in the elderly is under-recognized, particularly in primary care practices, general hospitals, and nursing homes.
The etiology of depression in the elderly is clearly multifactorial and several important contributory risk factors have been identified, including normal aging process, medical illnesses, chronic painful conditions, deficiency of essential nutrients, drug therapy, and psychosocial influences such as retirement, dependency, elderly neglect, death of spouse etc.
Elderly depression is different from depression of young and middle aged patients;
The following are certain symptoms of depression most commonly found in elderly.
- Agitation, anxiety
- Persistent, vague or unexplained physical complaints
- Memory problems; difficulty concentrating
- Social withdrawal, feelings of discouragement or hopelessness, inappropriate guilt
- Lack of attention to personal care
- Irritability and demanding behavior
- Prolonged grief after a loss
- Erratic sleep and appetite patterns.
- Suicidal thoughts or attempts.
- Depression may be early symptom of impending dementia & Parkinsonism.
Psychopathology of depression
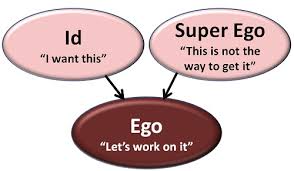
Psychoanalytical theory
In 1917 Sigmund Fraud wrote about mourning & Melancholia. Melancholic (Depression) is the response to either real (death of loved one) or perceived or symbolic (such as failure to achieve desired goal) event. A person’s unconscious anger or the loss leads to self hatred & self destructive behavior. According to him suicide is murder at 180 degree.
Behavioral theory
According to this theory depressive idea are learnt through experiences. This can be unlearnt through association & positive reinforcement.
Seligman suggests Learned helplessness (anaclitic depression) could play a role in the development of depression. The client fails to make any effort, because he strongly beleives that nothing could solve his problems making him fall helplessness & hopelessness.
Existential Theory
When a person keeps questioning his life, death, meaning of life & purpose of life he lapses into depression. Depression is characterized by a unique sense of hopelessness in feeling that his lives may actually be meaningless. People often have a limited awareness of themselves and the nature of their problem.
Gestalt Theory
Depression is seen in gestalt as unsatisfied needs. The seemingly lethargy of depression will if unblocked, be replaced by what it concealed and held in check –raging or the clonic movement of sobbing.
Neurochemistry of Depression
Studies have proved that in depressed individuals there are changes in certain neurotransmitters such as
- Serotonin,
- Nor epinephrine,
- Dopamine,
- GABA (Gamma amino butyric acid)
Other findings
- MRI and PET studies-Depressed individuals have reduced metabolism in left side of the brain, hippocampus, basal ganglia and thalamus
- Endocrine changes– elevated Hypothalamic pituitary adrenal (HPA)activity leading to Increase in cortisol, altered levels of prolactin, T3/T4, GH, CRF..,
- Changes in immune systems
- Alterations in sleep EEG (REM/NREM)
Course and prognosis
- Untreated Depression usually last for 1-6 months.
- 10-20% have chronic course (>2yrs)
- 30% will have recurrent episodes have two or more episodes.
- Up to 15% commit suicide
- With effective treatment up to 90% of patients can be symptom free
Management
- Before diagnosing Major Depression, other medical causes, the drug history, substance use should be evaluated.
- Base line investigations like complete blood counts, liver and renal function test, blood sugar, thyroid function tests, Ca2+, B12 levels should be checked.
- If any brain pathology is suspected CT/ MRI brain may be needed.
The line of management
- Antidepressants
- Psychotherapy
- ECT
Antidepressants
Antidepressants are the mainstay in treatment of depression. Studies have found that <25% of patients depression gets improved with a placebo (neutral drugs). While up to 60% of patients gets remitted with a single antidepressant.
Drugs are classified according to their mechanism of action in the brain.
- SSRI (Selective Serotonin Reuptake Inhibitor)
- TCA (Tricyclic Antidepressants)
- The dual acting drugs (SNRI) Serotonin Noradrenaline Reuptake Inhibitor
- The MAOIs
The SSRI’s
- Fluoxetine 20-60mg
- Sertraline 50-200mg
- Citalopram 20-40mg
- Escitalopram 10-20mg
- Paroxetine 10-40mg
These drugs are the first line of therapy and safe, and can be easily given to all ages and even during pregnancy.
The Tricyclics (TCA)
- Imipramine 25-225
- Amitriptiline 25-225
- Clomipramine 25-225
- Dothipen 25-225
These drugs are cheaper, highly effective, used in resistant depression, but their side effects like ant cholinergic side effects like constipation, dry mouth and sedation has reduced their use nowadays.
The dual acting drugs (SNRI)
- Venlafaxine 75-225mg
- Desvenlafaxine 50-200 mg
- Duloxetine 60-120mg
These drugs act to increase both serotonin and nor epinephrine in brain.
They are effective, comparatively less side effects but they are costly.
NASA (Mirtazipine) 7.5-45mg an effective sedative, antidepressant, anxiolytic with no sexual dysfunction
Monoamine oxidase inhibitor (MAO I) – Tranylcypromine 10-40 mg used in resistant anxiety and depressive disorders, but to be beware of hypertensive crisis and drug interactions, strict food control.
Treatment Resistant Depression (TRD)
If the usual line of management fails, or has partial remission, less than 50% improvement from the baseline.
Strategies to treat resistant depression
- Combination: relatively safe combination of antidepressants are tired SSRI + TCA: Sertraline 50-100mg and Imipramine 75-150mg solves most of the resistant depression
- Adjuvant with antipsychotics : low dose Olanzepine 2.5-5mg, Quetiapine 25-100mg, Amisulphride 50-100mg, Aripiprazole 2-10mg are effective add on to our routine antidepressants when the patient fail to remit usually, or when there is associated psychotic symptoms or agitation.
- Augmentation strategies: Lithium 0.4-0.8mEq/l (400-800mg), Thyroixne 25-100mmg, Bupropion 150-300mg , L-Methylfolate 15mg/day These are another class of drugs that aids in augmenting the antidepressant effect.
- Stimulants: Methylphenidate 10-20mg, Modafinil 100-200mg are psycho stimulants used in resistant or in patients with severe psychomotor retardation.
Non Invasive Brain Stimulation (NIBS)
Electro Convulsive Therapy (ECT)
One of the time tested effective method to treat depression, especially in patients with
- Suicidal ideations
- Severe psychomotor agitation or retardation
- Treatment resistant depression
- Severe depression with anorexia (significant weight loss, due to loss of appetite)
- Depression with catatonic symptoms
- Post partum depression at risk of infant and mother
- Severe depression with psychotic symptoms – with risk of suicide or violence
- Depression where the routine antidepressants fails or not tolerated
rTMS (repetitive Transcranial Magnetic Stimulation)
This is typically used when other medical management has not given expected results. This can be administered along with medication. The electro magnet painlessly delivers a magnetic pulse that stimulates nerve cells in the area of brain involves in mood control and depression. This is found to activate regions of the brain that function less in depression.
This treatment requires at least 20-30 sessions depending upon response over 3 months of period. There are very few side effects & it is one of the safest treatments.
Transcranial Direct Current Stimulation is a type of neuro modulation that uses constant low direct current (usually between 1 to 2 MA) delivered via electrodes on the skull. The electrodes are placed over fixed montages (T10 -20 system of EEG) that have been studied extensively for 30mts duration. 2 sessions /day with 3 Hrs intervals between are the current practice. Usually this is given for 5 days. But extended sessions are also being tried. This has absolutely no side effects. This is an effective add on therapy to regular antidepressant medicines.
When do patient improve?
- With medications it usually takes 6-8 weeks for remission (50% better) while for ECT patients can be much better within a week.
- Drugs have to be continued for at least a year after the full improvement.
- If there are more than 2 episodes or a strong family history of depression then drugs has to be given for life.
Psychotherapy
- These are a form of talk therapy where a trained therapist interacts with the patient, analyses them and their thinking modes, modifies the maladaptive thinking and behavior through gentle suggestion and examples.
- This usually takes 6-8weekly sessions each of 30-45 min.
- Their real advantage is it is devoid of side effects
- It is highly effective when combined with Pharmacotherapy
Three forms of psychotherapy commonly practiced in Depression
1. Cognitive Behavioral Therapy
Prof Aaron Beck introduced the CBT in Depression
Cognitive Behavioral Therapy (CBT) is a brief form of psychotherapy used in the treatment of adults and children with depression.
Its focus is on current issues and symptoms than people`s past history. CBT for depression involves several essential features: Identifying and correcting inaccurate thoughts associated with depressed feelings (cognitive restructuring), helping patients to engage more often in enjoyable activities (behavioral activation), and enhancing problem-solving skills.
The first of these components, cognitive restructuring, involves collaboration between the patient and the therapist to identify and modify habitual errors in thinking that are associated with depression.
Mindfulness Cognitive behavioral Therapy
Depressed patients often experience distorted thoughts about self (e.g. I am stupid- worthlessness), their environment (e.g. no one is helping me-helplessness) and their future (e.g. There is no sense in going forward, nothing will work out for me-hopelessness).
Information from the patient’s current experience, past history, and future prospects is used to counter these distorted thoughts.
The second component of CBT is behavioral activation where patients are encouraged to restart their activities that gave pleasure.
When patients are depressed, problems in daily living often seem unresolved. In the final process, the CBT therapist provides instruction and guidance in specific strategies for solving problems (e.g. breaking problems down into small steps).
Cognitive Behavioral Therapy is a scientifically well-established and effective treatment for depression. Over 75% of patients show significant improvements.
2. Mindfulness Cognitive behavioral Therapy
This therapy is based on the principles of Zen & Buddhism. Here in addition to regular CBT, also bringing in change in attitude- not to be judgmental, just live in the present the present (Mindfulness.)
Usually in depression, clients engage in automatic thoughts of the past that worsens the depression. The theory is to all activities consciously by aware of the present, avoiding automatic thoughts.
This therapy is very useful to prevention of relapse of depression. This is given predominantly in group setting over 8 weekly sessions.
3. Interpersonal Psychotherapy
Interpersonal Psychotherapy (IPT) is a short-term highly-structured type of psychotherapy with a strong focus on one area of interpersonal problems.
The main idea of this therapy is to look at the social functioning in one of 4 possible areas of life:
- Interpersonal Disputes- e.g. conflicts with spouse, with in-laws, higher officials.
- Role transitions – e.g. becoming a parent, promotion or de-promotion in job etc
- Grief- e.g. loss of a loved person
- Interpersonal deficits- e.g. lacking assertiveness, impulsivity etc.
The essentials during therapy are clarification, supportive listing, communication analysis, role playing, and encouragement of affect.
This process allows the patient to acknowledge the affective component of an interpersonal issue (e.g., grief) and helps the patient to accept it as a part of their experience.
The therapy is limited to not more than 12 or 16 one hour sessions.
Yoga and meditation
These have special importance in managing depression, a regular practice of simple warm up exercise, followed by basic Asanas and Pranayama helps to relive most of the depressive symptoms and even aimed at preventing depressive episodes
Meditation help in readjusting the altered HPA axis improve sleep and do control anger.
Spirituality: being spiritual calms one’s mind; patients are encouraged to follow their religious practice that they had earlier, while keeping educated about myths and reality.
Summary
- Depression is one of the commonest disorder, carries equal morbidity like that of a heart disorder.
- It requires early identification and the treatment is simple.
- The person’s quality of life and the overall social well being of the individual improves with appropriate treatment.
“Defeat Depression – Prevent Suicide”