Emergencies in Psychiatry
Psychiatric Emergencies that are seen in causality are
- Severe depression with agitation/psychotic symptoms/anorexia/suicidal ideations
- Acute psychosis
- Acute mania/ manic excitement in Bipolar disorder patients
- Catatonia
- Alcohol withdrawal and its complications
- Other drug abuse/withdrawal manifestations
- Grief and Bereavement
- Acute anxiety, Panic attack
- Dissociative disorders- Pseudo seizures, Possession episodes, Hyperventilation syndrome


10. Adolescent crisis
11. Intentional self-harm (ISH)
12. Child abuse – physical/sexual
13. Medications side effects of psychotropics
14. Psychological distress following an acute stress
In this section, we will discuss:-
- Aggression – due to various cause
- Side effects of psychotropic medications
- Catatonia
Aggressive/Exited /violent patient:
Behaviour intended to cause physical injury to self or others. The term may include a range of acts from verbal abuse to assault, either causing bodily injury or death or damage to property
- Up to 4-5% of the population are victims of violence in a given year.
- One in four women experiences domestic violence in their lifetimes.
- Violence is the 2nd leading cause of death in adolescence
Mental disorders and violence
It would be interesting to note that only 5% of prison inmates are mentally ill, and the rest had been imprisoned for the act done when they were “sane.”
Not all mentally ill are violent or aggressive
Most often, they are victims of violence.
Schizophrenia, Bipolar mania, acute psychoses are common disorders that lead to aggression/violence
Schizophrenia:
Patients under an actively psychotic episode can be aggressive at any time; also, he/she may be a victim of violence as well. A psychotic episode is a state where the patient loses reality yet oriented.
They may know whom they are targeting, with justification for themselves.
The lifetime risk for violence in schizophrenia is about 5 times that of the general population. Common in males, use of alcohol or other drugs.
Paranoid symptoms like delusions of reference, persecution, infidelity, the delusion of control are common causes.
In some cases, the patient may act to the command hallucinations.
The victims are usually known to the patient, such as family members or a neighbour.

An acute psychosis patient believed that his mother poisoned his food and attacked her when she insisted on eating. An alcoholic, who suspects his wife having illicit relationships with the neighbour, would either harm his wife or even assault the neighbour. A chronic schizophrenic patient slapped a shopkeeper because he heard a voice order to do so..,

Bipolar disorders- Mania
Patient during the heights of a manic episode is usually aggressive. The high self-esteem, high physical energy, irritable mood, grandiose beliefs, and hypersexual behaviour can all turn them violent at the person they encounter.
Often owing to their elated mood, they would consume alcohol or a similar substance, which adds up to the violence. Usually, they are either beaten up by the public or police for such activities before they are brought to a psychiatric hospital.
A 19 yr old boy, with a past history of mania 2 yrs ago, had been sleep-deprived during a current festival in his village found to be irritable, agitated, talking high, believed that he is the village deity (“Iyyanar”) found wandering his village with a huge billhook.
Substance use disorders:
Both withdrawal effects and intoxication of various substances can lead to belligerence behaviour. Intoxication leads to loss of inhibition, and the person becomes impulsive.
Withdrawal may be associated with severe craving, or the person who develops delirium may be violent.
Other disorders potential for violence:
Violence is common in certain personality disorders like antisocial PD or borderline PD.
People with learning disability, mental retardation violence may be found due to impaired ability to communicate, poor social and educational development.
Certain organic disorders like Delirium, Dementia, post head injury sequelae and Epilepsy are commonly associated with aggression.

Risk factors of violence
- Previous history of violence
- Unstable relationships
- Poor employment, disciplinary problems
- Substance misuse
- Personality disorders (paranoid, antisocial)
- childhood problems (conduct, abuse)
- Past Mental illness with violence
General principles in managing a violent patient
- Ensure the safety of self and other treating staffs
- Take help of significant others
- Keep away the person who the person is assaultive
- Introduce yourself to the patient: “sir, I’m Dr…,
- Call the patient by name, and explain the situation, orient him/her
- Provide them water to drink or feed them
- Tell the purpose of the interview “sir, you appear to be a bit agitated and anxious. We will calm you down with this medicine.”
Administer tranquillizers:
- The best and safest is Inj Lorazepam 2-4 mg IV slowly
- Inj Haloperidol 5-10mg IV/IM
- Inj Promethazine 50mg IM – which ensures sedation and prevents EPS form Haloperidol (to be avoided in delirious and demented patients)
Restrain: temporarily restraint is needed in some situation where the above drugs necessary time to act. Restrains should be made of gauze or soft cloths (not chains or belt), it should be 4 points, i.e., all the four limbs, upper limbs should be beside the body and lower ends to the ends of the cot. Once restrained, trained nursing staff should monitor the vitals, maintain hydration, and ease the patient.
Document all the above proceedings.
Collect more history, order relevant investigations and ascertain a diagnosis.

Legal implications of violence:
A patient with a history of mental illness committed a crime and brought by police
Here we have to access
- Whether the patient was mentally ill during such a crime
- Whether the patient was aware of the action during the crime
- What was the patient explanation of the act of crime
- Whether the patient aware of its complications
- Whether the patient aware that the act is against the law
we could prove to the court of law the above three we can save the patient from punishment
The M’Naghten rule (pronounced, and sometimes spelt, McNaughton) is any variant of the 1840s jury instruction in a criminal case when there is a defence of insanity:
that every man is to be presumed to be sane, and … that to establish a defence on the ground of insanity, it must be clearly proved that, at the time of the committing of the act, the party accused was labouring under such a defect of reason, from a disease of the mind, as not to know the nature and quality of the act he was doing; or if he did know it, that he did not think he was doing what was wrong
Establishing Insanity
Currently, states rely on four different tests to determine whether a defendant is legally insane. The laws of your state will establish which of these four tests applies.
Under the M’Naghten Rule test, the criminal defendant must either not understand what they did or be unable to distinguish right from wrong. This test relies on the notion that defendants may be diseased such that they are incapable of understanding their own actions.
The Durham Rule holds that if a criminal defendant’s “mental disease or defect” was why he or she committed a crime, the defendant is not guilty because of insanity. This test is currently used only in New Hampshire since it has been deemed too broad by other states and jurisdictions.
The irresistible impulse test is used to determine whether, as a result of mental disease or defect, a defendant could not control or resist his or her own impulses, thus leading to a criminal act. If so, the defendant is not guilty because of insanity. Some states consider this test combined with the M’Naghten test, holding that when a defendant could not understand his or her own actions, nor control them, the insanity defence applies.
Under the Model Penal Code, the insanity defence applies when, because of a diagnosed mental disorder, the defendant could not understand the criminality of his or her actions or was unable to “act within the confines of the law.” This test is still used in many states, but it was criticized after it led to John Hinckley’s acquittal.
- Stupor and Catatonic Syndrome
Catatonia is characterized by abnormal motor behaviour, with periods of hyper and hypoactivity usually associated with mutism and stupor.
Common features of catatonia are
- Negativism: motiveless resistance to all instructions or maintenance of a rigid posture against attempts to be moved
- Automatic obedience: a robot-like response to any instruction, however silly.
- Mutism: does not communicate either through speech or even gestures.
- Posturing: They sometimes hold rigid poses for hours called Posturing and will ignore any external stimuli.

- Psychological pillow: They often lie in bed with head partially raised as if they are resting on a pillow called “Psychological pillow”.
- Stereotypy: There may also show repetitive movements, like a military salute, praying or prostrating to everyone.
- Grimacing: unusual facial movements like squinting eyes, pooping out mouth or tongue
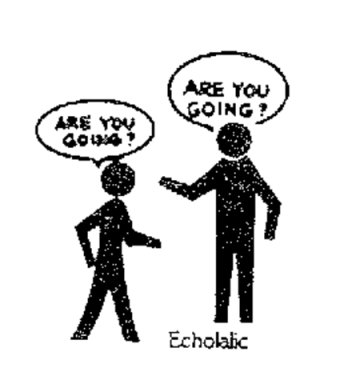
- Echolalia & Echopraxia: They may repeat meaningless phrases or speak only to repeat what the examiner says called Echolalia, similarly imitating actions of others called Echopraxia.
Differential diagnosis: catatonia can be due to a psychiatric aetiology or organic (neurological or even medical cause)
Psychiatric disorders
- Depression with/without psychotic symptoms
- Schizophrenia, acute psychosis
- Mania
Organic (neurological)
- Post-encephalitic Parkinsonism
- Limbic encephalitis
- Subacute sclerosing panencephalitis (SSPE)
- Petit mal seizures
- The post-ictal phase of epilepsy
- Carbon monoxide poisoning
Two types of catatonia:
- Stupor is a motionless, apathetic state in which one is oblivious or does not react to external stimuli. Motor activity is nearly non-existent. Individuals in this state make little or no eye contact with others and maybe mute and rigid.
- Catatonic excitement is the state of constant purposeless agitation and excitation. Individuals in this state are extremely hyperactive, although the activity seems to lack purpose.
“If left untreated, these patients may die of hypoglycemia or exhaustion”.
Management
Routine blood investigations, especially blood sugar, toxin/drug screen, EEG, CSF analysis, CT brain may be necessary to rule out any organic pathology.
The Initial treatment is aimed at providing relief from the catatonic state. A test dose of 1-2 mg intramuscular lorazepam will often result in marked improvement within half an hour, which is diagnostic to confirm its catatonia.
The treatment aimed at finding the underlying cause, once Psychiatric diagnosis is confirmed
ECT is the best choice which brings down the patient into normalcy within one or two treatments. Patients are after that interviewed and differentiated between the psychotic or depressive form of catatonia.
Drug-induced side effects
Neuroleptic drug-induced Extrapyramidal symptoms (EPS)
Acute dystonia is an emergency where the patient presents with acute, sustained, painful muscle spasm producing twisted abnormal postures. Ex: sudden deviation of jaw, neck, hand.., Caused by high doses of typical antipsychotics like Haloperidol, trifluoperazine, chlorpromazine
Newer drugs like Risperidone can also cause it. Drugs like olanzapine, quetiapine, clozapine practically do not cause dystonia.
Treatment is administered IM injection of promethazine (Phenergan), followed by oral Trihexyphenidyl, reduction of the causative antipsychotic, or replacing with atypical drugs olanzapine or quetiapine.

Drug-induced Parkinson’s syndrome:
It is characterized by tremor, rigidity and bradykinesia, drooling of saliva, gait disturbances, blunt affect.
Typical and atypical drugs cause it at higher doses, caused by excessive D2 blockade in the nigrostriatal pathway, leading to an imbalance between dopamine and acetylcholine in this pathway.
Treatment is either reducing the dose or switching to another atypical antipsychotic agent like olanzapine or quetiapine.
Adding anticholinergic agents like Trihexyphenidyl 2mg BID (PACITANE)
Drug-induced Akathesia:
This is an unpleasant and distressing side effect of antipsychotic treatment, especially with typical and some atypical (newer) drugs.
Patients are markedly restless and agitated walking to and fro. Typically, the patient may report a SUBJECTIVE FEELING OF INNER RESTLESSNESS.
Caused by an imbalance between Noradrenaline and Dopamine neurotransmitters.
Prevention: slow titration of antipsychotic drugs.
Treatment: reduction of the offending drug.
Add
- Propranolol 20mg TID
- Lorazepam 1-2mg TID
- Trihexphenidyl 2mg BID
Neuroleptic Malignant Syndrome (NMS)
This is rather serious neuromuscular dysfunctions, found with higher doses of antipsychotics, repeated IM /IV injections.
A patient would have altered sensorium, high-grade fever(up 107 F), tachycardia, tachypnoea, hypo/hypertension, diaphoresis, tremors, generalized rigidity, incontinence, metabolic acidosis and renal failure.
Blood investigations: Leukocytosis, myoglobinuria, increased urea /creatinine.
Treatment: stop the antipsychotics, admit pt in ICU care, supportive nutrition, fluid and electrolyte balance, Inj Dantrolene (calcium channel blocker) muscle relaxant.
If not diagnosed or delayed management -the mortality rate is up to 20%.